Comprehensive Medical Care For Diabetes
Comprehensive medical care for diabetes is the care for diabetes patients from the time of diagnosis of disease, this includes glycemic control, medications, lifestyle management including diabetes self-management education and support, nutrition therapy, physical activity and psychological care and also detection and management and prevention diabetes mellitus specific complications and modifying risk factors for diabetes mellitus associated diseases.
The care is patient-centred and individualized as advocated by the American diabetes association.
Who is in the diabetes care team?
The diabetes care team involves a multidisciplinary group of healthcare professionals who are available to support the person with diabetes, Members of the diabetes care team usually include the primary care provider and/or the endocrinologist or diabetologist, a certified diabetes educator, a nutritionist, a psychologist, and possibly a social worker. In addition, when the complications of diabetes mellitus arise, subspecialists (including ophthalmologists, neurologists, podiatrists, nephrologists, cardiologists, and cardiovascular surgeons) with experience in diabetes mellitus-related complications are essential.
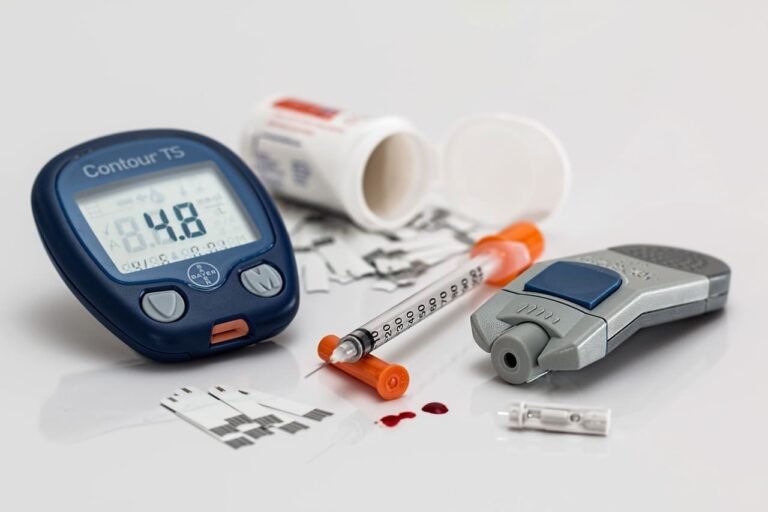
How to self-assess glycaemic control?
It’s a short-term measure of capillary blood glucose by glucose monitors using a small drop of blood obtained from the fingertip. The frequency of measurement according to the type of diabetes, Patients with type 1 diabetes should test capillary blood glucose 4 or more times per day as they usually require intensive insulin regimens. Patients with type 2 diabetes usually only need to self-test capillary blood glucose regularly if they require insulin or sulphonylurea therapy. For those on insulin, blood glucose testing 1–4 times daily (depending on the intensity of the prescribed regimen) helps guide insulin dosing and manage diet, exercise, and illness. It also helps detect and protect against hypoglycaemia.
This is also the case for sulphonylurea therapy. People with type 2 diabetes who are on neither of these therapies do not have an absolute need to test blood glucose, but it can be useful, e.g. for self-education on the effects of food and exercise on glycaemia( blood suger levels).
How to assess long-term glycemic control?
Measurement of glycated hemoglobin (HbA1c) is the standard method for assessing long term glycemic control. When plasma glucose is consistently
elevated, this alteration reflects the glycemic history over the previous 2–3 months,
because red blood cells have an average life span of 120 days. Measurement of HbA1c allows for more rapid feedback and may therefore assist in the adjustment of therapy. HbA1c should be measured in all individuals with diabetes mellitus during their initial evaluation and as part of their comprehensive diabetes care. As the primary predictor of long-term complications of diabetes mellitus.
What is continuous glucose monitoring (CGM)?
CGM technology utilizes a sensor or electrode to detect interstitial glucose, which is in equilibrium with blood glucose, but may lag when the blood glucose is changing. In one CGM approach, the interstitial glucose is detected and reported essentially continuously while in another approach, the sensor is in place, but the glucose is only recorded when a detector is placed over the sensor. The glucose sensors are placed subcutaneously and are replaced every 3–14 days. CGM also allows the patient to monitor the rate of glucose change and glucose trends that can be used to avoid predicted hyper- or hypoglycemia. CGM in type 1 diabetes mellitus especially in those with hypoglycemia unawareness can decrease the
frequency of serious hypoglycemia (especially nocturnal hypoglycemia).

How to diet in diabetic patients?
Diet plays an important role in the effective management of type 1 diabetes and type 2 diabetes and is fundamental to the prevention of type 2 diabetes. Diet management of diabetes aims to optimize glycaemic and blood pressure management, correct any lipid abnormalities, and, in doing so,
reduce the risk of long-term complications. In general, the dietary management is similar for individuals with type 1 or type 2 diabetes mellitus—high-quality, nutrient-dense with limits on carbohydrate intake required for glycemic control and weight management, but dietary advice must be evidence based and individualized, taking into account personal and cultural preferences, and ensuring the diet is appropriate and compatible with the person’s lifestyle, existing treatment regimen, other comorbidities, and willingness to change.
All diabetic patients should eat most of these: whole, unprocessed, non-starchy vegetables, Non-starchy vegetables like lettuce, cucumbers, broccoli, tomatoes, and green beans have a lot of fiber and very little carbohydrate, which results in a smaller impact on your blood sugar. Remember, these should make up half your plate.
Eat some of these: whole, minimally processed carbohydrate foods. These are your starchy carbohydrates, and include fruits like apples, blueberries, strawberries and cantaloupe; whole intact grains like brown rice, whole wheat bread, whole grain pasta and oatmeal; starchy vegetables like corn, green peas, sweet potatoes, pumpkin and plantains; and beans and lentils like black beans, kidney beans, chickpeas and green lentils.
Eat less of these: refined, highly processed carbohydrate foods and those with added sugar. These include sugary drinks like soda, sweet tea, and juice, refined grains like white bread, white rice, and sugary cereal, and sweets and snack foods like cake, cookies, candy, and chips.
What are the benefits of exercise in diabetics?
Exercise has multiple positive benefits including cardiovascular risk reduction, reduced blood pressure, maintenance of muscle mass, reduction in body fat, and weight loss. For individuals with type 1 or type 2 diabetes mellitus, exercise is also useful for lowering plasma glucose (during and following exercise) and increasing insulin sensitivity. People with type 1 diabetes (and people with insulin-treated type 2 diabetes) face additional challenges with exercise compared with the general population due to the risk of exercise-induced hypoglycaemia,
To avoid exercise-related hyper- or hypoglycemia, individuals with type 1 diabetes mellitus should :
- Monitor blood glucose before, during, and after exercise
- Delay exercise if blood glucose is >14 mmol/L (250mg/dL) and ketones are present
- If the blood glucose is <5.0mmol/L (90 mg/dL), ingest carbohydrate before exercising
- Monitor glucose during exercise and ingest carbohydrate as needed
to prevent hypoglycemia - Decrease insulin doses (based on previous experience) before and after exercise and inject insulin into a non-exercising area
- learn individual glucose responses to different types of exercise
What are the benefits of Weight management in diabetics?
Central obesity with increased waist circumference is particularly associated with insulin resistance and increased cardiovascular risk so weight loss markedly improves glycaemic control and slows diabetes progression. It has beneficial effects on HbA1c. Substantial weight loss in obese people (usually around 15 kg or about 15% initial body weight) can put type 2 diabetes into remission.
What are the effects of alcohol on diabetics?
In type 1 diabetes (and for people with insulin-treated type 2 diabetes) alcohol can also reduce hypoglycaemia awareness and suppress gluconeogenesis, increasing the risk of hypoglycaemia. In addition, the signs of hypoglycaemia can be mistaken for alcohol intoxication by observers. People with insulin-treated diabetes are there fore advised during ingestion of alcohol to:
- let a companion know that they have diabetes and how to treat them if they have hypoglycaemia
- continue to monitor and correct blood glucose by eating while drinking
- measure and ensure glucose is not low before retiring to bed
How to drive safely for diabetics?
People with diabetes who take insulin therapy must have adequate awareness of
hypoglycaemia, have had no more than one episode of hypoglycaemia in the preceding 12 months, In addition, Blood glucose levels should be over 5.0mmol/L (90mg/dL) before driving; if they are below 4.0mmol/L (72mg/dL) or there are symptoms of hypoglycaemia the person should not drive.
Insulin-treated drivers should:
- Blood glucose testing is required to be performed no more than 2hours before the start of a journey and every 2hours while driving.
- Keep an accessible supply of fast-acting carbohydrate in the vehicle
- Take regular snacks or meals during long journeys
- Stop driving if hypoglycaemia develops
- Pull over and sit in the passenger seat
- Wait 45 minutes after correction of hypoglycaemia before resuming driving (delayed recovery of cognitive function)
- Carry identification in case of injury
What is the advice for diabetics in Ramadan?
People with diabetes should schedule a visit with a diabetes health-care professional 6–12 weeks before Ramadan for dissections and education around fluids and meal planning, when to exercise, the role of increased frequency and/or timing of glucose monitoring(which does not invalidate the fast) and adjustment to the dose time and/or frequency of glucose-lowering agents. The majority of people with type 2 diabetes can be supported to fast during Ramadan provided they are prepared to stop the fast in the case of frequent hyper- or hypoglycaemia or worsening of other related medical conditions. While people with type 1 diabetes are advised not to fast, this advice should be considered on a case by-case basis. The highest risk of hypoglycaemia is in people who are managed with
sulphonylureas and insulin (especially if they are older age, or have renal failure or
advanced macrovascular complications); such individuals need careful blood glucose monitoring and, if necessary, their treatment regimens may need to be adjusted.