Diabetes Mellitus: What It Is, Types, Causes, Complications&Treatment
wHAT Is DIABETES MELLITUS?
Diabetes mellitus (DM) is a clinical syndrome that affects any system in the body which is characterised by the presence of high sugar levels in the blood (mellitus being Latin for sweet) which is due to either absolute insulin deficiency (type 1 DM) or relative insulin deficiency (type 2 DM).
What are type 1 and type 2 diabetes mellitus?
Type 1 DM is approximately 5% of all diabetic patients, It’s characterised by severe
deficiency of insulin, patients require insulin to live, The onset is typically in youth (before 20 years), but can occur at any age.
Type 2 DM accounts for 90% or more of all diabetic patients, The insulin levels are usually normal to high but may diminish over many years of having diabetes because there is reduced sensitivity to insulin in peripheral tissue (due to obesity) which is called insulin resistance.
What is the Pathogenesis of type 1 diabetes mellitus?
Type 1 DM is the result of interactions of genetic, environmental, and immunological factors that ultimately lead to immune-mediated (autoimmune) destruction of the pancreatic beta cells and insulin deficiency, In susceptible individuals, the autoimmune process is thought to be triggered by an infectious or environmental stimulus. In the majority of patients, autoantibodies against beta cell antigens appear after this triggering event, followed by progressive loss of insulin secretion, The rate of decline in beta cell function varies widely among individuals, with some patients progressing rapidly to clinical diabetes and others
evolving to diabetes more slowly and over several years.
What is the Pathogenesis of type 2 diabetes mellitus?
- Obesity is a major cause of insulin resistance, Intra-abdominal ‘central’
Adipose tissue is metabolically active and releases large quantities of free fatty acids (FFAs), which may induce insulin resistance because they compete with (or inhibit use of) glucose as a fuel supply for oxidation, e.g. in muscle. In addition, adipose tissue releases several hormones (including a variety of peptides, called ‘adipokines’) that act on specific receptors to influence
Sensitivity to insulin in other tissues. Examples of adipokines include leptin, adiponectin, interleukin-6, and tumour necrosis factor alpha. - Genetics: mutations in the insulin receptor cause diabetes due to severe insulin resistance (e.g. Rabson–Rabson-Mendenhall and Donohue syndromes); such individuals hava functional effect via an abnormal receptor.
- Age: insulin production decreases with age.
What are the Causes and risk factors for type 1 D?
- Genetic factors
- Central obesity
- Ethnicity
- Reduced physical activity
- Hormone excess, Excess endogenous production of hormonal antagonists to insulin, e.g:
- Growth hormone – acromegaly
- Glucocorticoids – Cushing’s syndrome
- Glucagon – glucagonoma
- Catecholamines – phaeochromocytoma
- Thyroid hormones – thyrotoxicosis
- Drug-induced (e.g. glucocorticoids, thiazide diuretics, HIV drugs, immune checkpoint inhibitors)
- Associated with genetic syndromes (e.g. Down syndrome, Klinefelter syndrome, Turner syndrome, DIDMOAD (Wolfram syndrome), Friedreich’s ataxia, myotonic dystrophy)
What are the Causes and risk factor fore type 2 diabetes mellitus?
- Genetic factors
- Increasing age
- Pancreatic pathology (e.g. pancreatitis, pancreatectomy, neoplastic disease, cystic fibrosis, haemochromatosis, fibrocalculous pancreatopathy)
- Toxins, e.g. alcohol, cytokines
- Infections, e.g. SARS-CoV-2
- Glucotoxicity
- Lipotoxicity
- Deposition of islet amyloid polypeptide

What are the symptoms of diabetes mellitus?
- Polyuria(increased frequency of urination) due to the glucose in the renal tubules causes osmotic retention of water, causing a diuresis
- Polydipsia(thirst) and dry mouth due to a physiological response to diuresis to maintain plasma volume
- Hyperphagia (predilection for sweet foods)
- Tiredness, nausea, and headache
- Weight loss due to loss of anabolic effects of insulin
- blurred vision caused by swelling of the lens due to osmosis (caused by increased glucose)
- Mood change, irritability, difficulty in concentrating, and apathy
- Fungal infection of the mouth and vagina due to decrease of immunity
- Numbness, tingling of hands and feet due to neuropathy
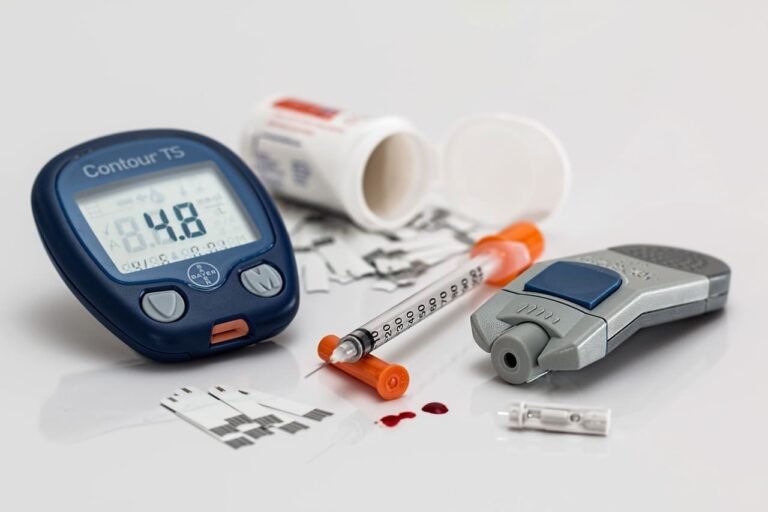
How is diabetes mellitus diagnosed?
Diabetes is confirmed by international consensus as:
- Random plasma glucose test ≥11.1 mmol/L (200 mg/dL)
- Fasting plasma glucose ≥7.0 mmol/L (126 mg/dL) on two occasion
- Haemoglobin A1c ≥48 mmol/mol (>6.5%)
What is pre-diabetes?
Impaired fasting glucose:
- fasting plasma glucose ≥6.1 mmol/L (110 mg/dL) and <7.0 mmol/L(126 mg/dL) (World Health Organization)
- fasting plasma glucose ≥5.6 mmol/L (100 mg/dL) and <7.0 mmol/L (126 mg/dL) (American Diabetes Association).
Impaired glucose tolerance: - plasma glucose <7.0 mmol/L (126 mg/dL) and 2-hr glucose after 75 g oral glucose drink ≥7.8 (140 mg/dL) and <11.1 mmol/L (200 mg/dL).
Hemoglobin A1c: - 42–47 mmol/mol (National Institute for Health and Care Excellence [NICE] guidelines, UK)
- 39–47 mmol/mol (American Diabetes Association)
What are the acute complications of diabetes mellitus?
Diabetic ketoacidosis (DKA) and Hyperglycaemic hyperosmolar state (HHS) are acute, severe disorders directly related to diabetes. DKA was formerly considered a hallmark of type 1 DM, but it also occurs in individuals with type 2 DM who can sometimes subsequently be treated with oral glucose-lowering agents.
HHS is primarily seen in individuals with type 2 DM. Both disorders
are associated with absolute or relative insulin deficiency, volume depletion, and acid–base abnormalities. DKA and HHS exist along a continuum of hyperglycemia, with or without ketosis. Both disorders are associated with potentially serious complications if not promptly diagnosed and carefully treated. Another important acute complication of diabetes mellitus is hypoglycaemia caused by insulin and insulin-producing drugs used to treat diabetes mellitus or by exposure to other drugs including alcohol.
What are the chronic complications of diabetes mellitus?
Diabetes-related complications can be divided into vascular and nonvascular
complications, which are similar for type 1 and type 2 DM. The vascular complications of DM are further subdivided into microvascular (retinopathy, neuropathy, nephropathy) and macrovascular (coronary heart disease, peripheral arterial disease, cerebrovascular disease) complications.
Nonvascular complications include infections, skin changes, hearing loss, and increased risk of dementia and impaired cognitive function.
What is the treatment for diabetes mellitus?
The aims for both types 1 and 2 diabetes:
- Initially to reduce blood sugar levels and relieve related symptoms
- Minimise the risks of long-term microvascular and macrovascular complications
- Allow the patient to achieve as normal a lifestyle as possible
Comprehensive care of type 1 and type 2 DM requires an emphasis on nutrition, exercise, and monitoring of glycemic control (as a part of comprehensive medical care for diabetes) but also usually involves glucose-lowering medication(s). The usual target HbA1cis < 7.o%(53 mmol/mol)for both type 1 and type 2 diabetes but as recommended by
the American diabetes association Treatment goals of glycemic control for diabetic patients should be individualized for each patient according to: - The patient’s age and ability to understand and implement a complex treatment regimen
- Presence and severity of complications of diabetes
- known CVD(cardiovascular diseases)
- Ability to recognize hypoglycemic symptoms
- Presence of other medical conditions or treatments that might affect survival or the response to therapy
- lifestyle and occupation (e.g., possible consequences of experiencing hypoglycemia on the job), and level of support available from family and friends.
Microvascular complications are prevented by targeting hyperglycaemia, but control of macrovascular complications also requires management of associated risk factors, particularly hypertension, dyslipidaemia, and cigarette smoking. Due to the risk of complications, people with all forms of diabetes
should be kept under review with regular monitoring, adjustment of treatment, and screening to detect treatable complications as early as
possible. Click here to read more details about the treatment of type 1 diabetes and type 2 diabetes