Diabetic ketoacidosis: What Is, Causes, Signs&Symptoms
What is Diabetic ketoacidosis?
Diabetic ketoacidosis is an acute metabolic complication of diabetes mellitus which is a life-threatening medical emergency that can occur in both type 1 and type 2 diabetic patients but is more common in type 1 diabetes.
What is the pathogenesis of DKA?
DKA results from relative or absolute insulin deficiency combined with counter-regulatory hormone excess ( glucagon, catecholamines, cortisol, and growth hormone). Both insulin deficiency and glucagon excess, in particular, are necessary for DKA to develop. The decreased ratio of insulin to glucagon promotes gluconeogenesis, glycogenolysis, and ketone body formation in the liver, as well as increases in substrate delivery from fat and muscle (free fatty acids, amino acids) to the liver. Ketosis results from a marked increase in free fatty acid release from adipocytes, with a resulting shift toward ketone body synthesis in the liver.
What are the signs & symptoms of DKA?
- Nausea and vomiting
- Polyuria, thirst
- Abdominal pain (more common in children) that may mimic acute abdomen often with guarding and rigidity
- Kussmaul respiration (rapid, deep breathing)
- Fruity” (acetone) breath odor
- Marked dehydration, hypotension (postural or supine), tachycardia
- Cold extremities/peripheral cyanosis
- Altered consciousness, drowsiness, and frank coma may occur if not treated
What are the precipitating factors for DKA?
- Inadequate insulin administration
- Infection (pneumonia, urinary tract infection, gastroenteritis, sepsis)
- Infraction (cerebral, coronary, mesenteric, peripheral)
- Pancreatitis
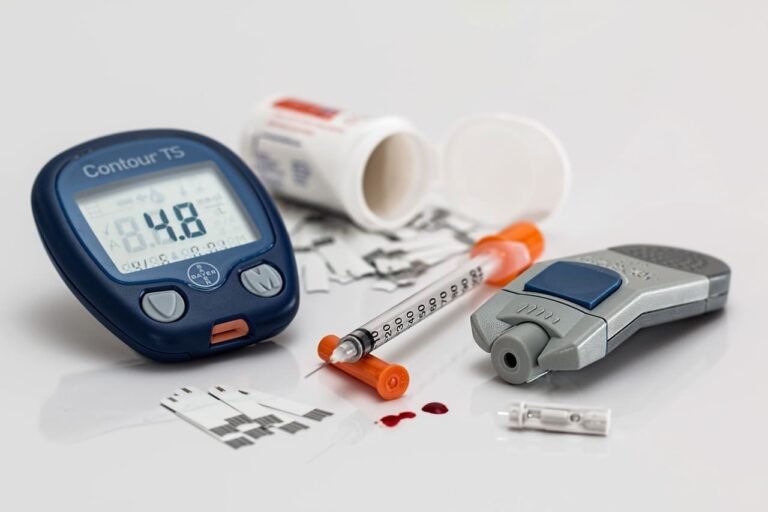
How is DKA diagnosed?
- Hyperglycemia: serum glucose typically >450 mg/dL and <850 mg/dL (in certain conditions, e.g., alcohol ingestion, the patient may be euglycemic)
- Metabolic acidosis:Blood pH <7.3 and serum HCO3− <15 mEq/L, Increased anion gap—due to production of ketones (acetoacetate and βhydroxybutyrate)
- Ketonemia (serum positive for ketones) and ketonuria
- Serum levels of acetoacetate, acetone, and β-hydroxybutyrate are greatly increased
- Hyper-osmolarity
- Hyponatremia—Serum sodium decreases 1.6 mEq/L for every 100 mg/dL increase in glucose level because of the osmotic shift of fluid from the ICF(intracellular fluid)to the ECF(extracellular fluid) space. Total body sodium level is normal. This generally does not require treatment
- Hyerkalemia because of the acidosis, hyperkalemia may be present initially, although total body potassium is low. As insulin is given, it causes a shift of potassium into cells, resulting in hypokalemia, and this can happen very rapidly
- Phosphate and magnesium levels may also be low
What are the complications of DKA?
With appropriate therapy, the mortality rate of DKA overall is (0.2%-2%) and is related more to the underlying or precipitating event, such as infection or myocardial infarction, and else. The major nonmetabolic complication of DKA therapy is cerebral edema, which most often develops in children as DKA is resolving. The
etiology of and optimal therapy for cerebral edema is not well established, but
over replacement of free water and rapid normalization of serum glucose should be avoided.
what is treatment of dka?
Treatment of DKA includes insulin, fluid, and potassium
Insulin:
- Give insulin immediately after the diagnosis is established.
- Give a priming dose of 0.1 units/kg of regular insulin (IV) followed by an infusion of 0.1 units/kg per hour. This is sufficiet to replace the insulin deficit in most patients, but should be ensure that patient is not hypokalemic before giving insulin.
- Continue the insulin until the anion gap closes and metabolic acidosis is corrected, then begin to decrease the insulin. Give SC (subcutaneous) insulin when the patient starts eating again.
Fluid replacement (normal saline):
- Give fluids immediately after the diagnosis is established.
- Add 5% glucose once the blood glucose reaches 250 mg/dL to prevent hypoglycemia.
potassium replacement:
- Replace potassium prophylactically with IV fluids.
- Initiate within 1 to 2 hours of starting insulin.
- Ensure adequate renal function (urine output) before administering these.
- Monitor potassium, magnesium, and phosphate levels very closely and replace as necessary.