Hyperglycaemic Hyperosmolar State: What IS, Causes, Symptoms, Diagnosis
what is Hyperglycaemic hyperosmolar state?
Hyperglycaemic hyperosmolar state (HHS) is a medical emergency that is a consequence of prolonged relative insulin deficienc that is typically seen in elderly with type 2 diabetes mellitus patients.
what is Pathogenesis of HHS?
Hyperglycaemic hyperosmolar state results from relative insulin deficiency and inadequate fluid intake are the underlying causes of HHS. Insulin deficiency increases hepatic glucose production (through glycogenolysis and
gluconeogenesis) and impairs glucose utilization in skeletal muscle. Hyperglycemia induces an osmotic diuresis that leads to intravascular volume depletion, which is exacerbated by inadequate fluid replacement. Ketosis and acidosis are typically absent or minimal which can differentiate it from diabetic ketoacidosis.
what are Precipitating factors for hhr?
- -Any type of stress or illness (e.g., infectious process, trauma, myocardial infarction, stroke, recent surgery, sepsis, GI bleeding).
- Inadequate fluid intake (either due to lack of access in elderly/bedridden or to inadequate thirst drive) to keep up with urinary fluid losses due to continued hyperglycaemic (osmotic) diuresis.
WHAT ARE Signs & Symptoms OF HHS?
- Thirst, polyuria
- severe dehydration, hypotension, and tachycardia
- Focal neurological signs (e.g; seizure) secondary to hyerosmolarity
- Lethargy and confusion may develop leading to coma
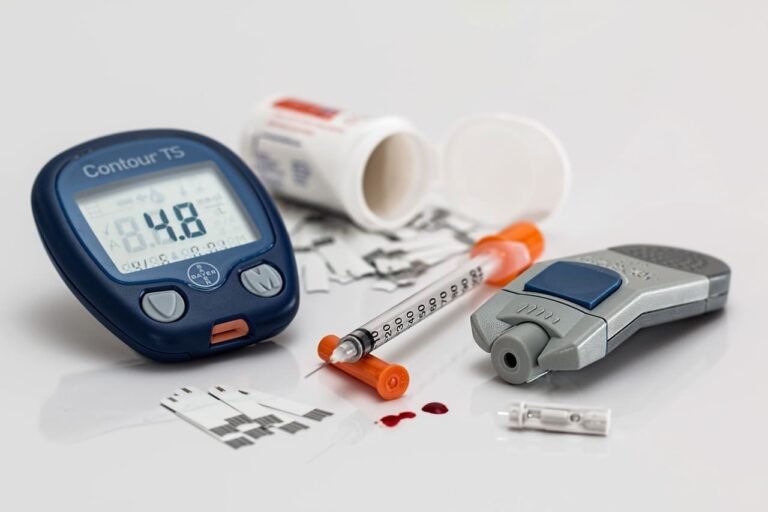
How is HHS diagnosed?
- severe hyperglycaemia, plasma glucose > 55.5mmol/L(1000mg/dL)
- Hyerosmolarity > 350mOsmol/L
- BUN (blood urea nitrogen), pre-renal azotemia is common
- Serum pH >7.3 (no acidosis), serum HCO3- > 15
WHAT IS TREATMENT OF HHS?
- Fluid replacement (normal saline): 1 L in the first hour, another liter in the next 2 hours. Most patients respond well. Switch to half-normal saline once the patient stabilizes.
- When glucose levels reach 250 mg/dL, add 5% glucose (D51/2NS) as in
DKA. - In patients with cardiac disease or renal insufficiency, avoid volume overload
(can lead to CHF), but generous fluids are still needed. - Insulin: An initial bolus of 5 to 10 units intravenously, followed by a continuous low-dose infusion (2 to 4 units/hr) is usually appropriate