Hypoglycaemia(low blood suger): What IS, Causes, Symptoms, Treatment
what is hypoglycaemia(low blood suger)?
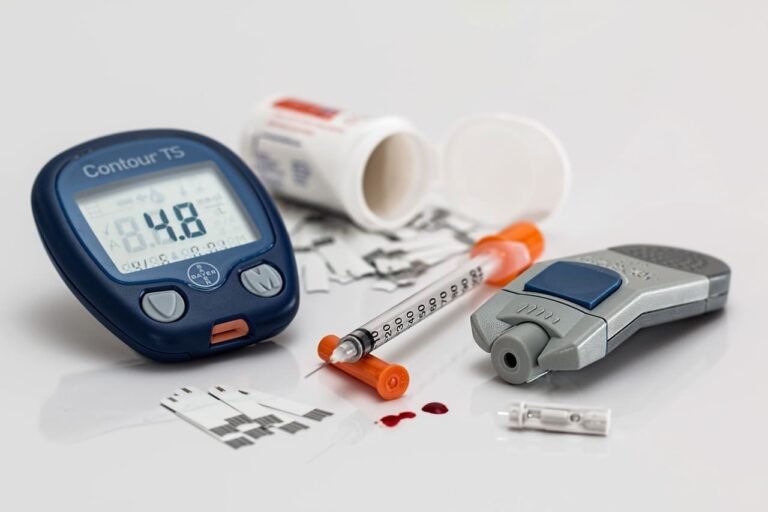
Hypoglycaemia is defined as blood sugar levels <70mg/dL(3.9mmol/L), the most
commonly caused by insulin or insulin production drugs used to treat diabetes mellitus or by exposure to other drugs including alcohol. Hypoglycaemia can be documented by Whipple ś triad:
- Symptoms consistent with hypoglycaemia
- Low blood glucose measured at the time of symptoms
- Symptoms resolved on correction of hypoglycaemia
What are the physiological responses to hypoglycaemia?
- -Decrees insulin secretion by the pancreas ( first defense against hypoglycaemia)
- Increase glycogon (second defense against hypoglycaemia
- Increase epinephrine (third defense against hypoglycaemia critical when glycogon is deficient
- Increase cortisol and growth hormone (involved in defense against prolonged
hypoglycaemia) - Decrease cognition (symptoms promote behavioural defense against hypoglycaemia critical, including the ingestion of food)
Hypoglycaemia
Excess insulin:
-
Erroneous injection of insulin (e.g. dose miscalculation or injection of incorrect
insulin type) -
Lipohypertrophy at injection sites (causing variable insulin absorption)
-
Bariatric surgery (can cause hyperinsulinaemia)
Increased sensitivity to insulin:
- Exercise
- Weight loss
- Sudden reduction in glucocorticoids
- Unrecognised Addison’s disease
Reduced carbohydrate intake/increased metabolic demand:
- Irregular or missed meal
- Gastroparesis due to autonomic neuropathy causing variable carbohydrate
absorption - Bariatric surgery
- Malabsorption, e.g. coeliac disease
- Eating disorder
- Early pregnancy
- Breast feeding
Reduced gluconeogenesis and/or glycogen reserves:
- Alcohol
- Chronic kidney disease
- Advanced liver disease
Increased glucose variability:
- Absent/minimal endogenous insulin secretion (reduced C-peptide)
- Long-duration type 1 diabetes/insulin-treated type 2 diabetes
- Young age of onset of type 1 diabetes
- Impaired awareness of hypoglycaemia
- Rapid improvement in and/or strict glycaemic control
- Previous severe hypoglycaemia
- Long-duration type 1 diabetes/duration of insulin-treated type 2 diabetes
- Older age
- Dementia
- Sleep
- No or inadequate glucose monitoring
What are the symptoms of hypoglycaemia?
- Autonomic symptoms(Sweating, Trembling, Pounding heart, Hunger, and Anxiety ) result from the perception of physiologic changes caused by the central nervous system–mediated sympathoadrenal discharge that is triggered by hypoglycemia.
- Neuroglycopenic symptoms (Delirium, Drowsiness, Speech difficulty, Inability to concentrate, Incoordination Irritability, and anger) result from central nervous system glucose deprivation.
- Others Non-specific symptoms (Nausea, Tiredness, Headache).
How is hypoglycaemia diagnosed?
- Level 1 hypoglycaemia (alert value) as <3.9 mmol/L(<70 mg/dL) but ≥3.0 mmol/L(≥54mg/dL).
- Level 2 hypoglycaemia (clinically significant ) is diagnosed as <3.0 mmol/L (<54 mg/dL).
- Level 3 hypoglycaemia (severe) is diagnosed as any low blood glucose level leading to cognitive impairment and the need for external assistance to provide glucose, glucagon, or other corrective activity.
what is treatment of hypoglycaemia?
- If the patient is able and willing, oral treatment with glucose tablets or glucose-containing fluids, candy, or food is appropriate. A reasonable initial dose is 15–20 g of glucose.
- If the patient is unable or unwilling (because of neuroglycopenia) to take carbohydrates orally, parenteral therapy is necessary. IV administration of glucose (25 g) should be followed by a glucose infusion guided by serial plasma glucose measurements. If IV therapy is not practical, SC or IM glucagon (1.0 mg in adults) can be used, particularly in patients with type 1 diabetes mellitus. Because it acts by stimulating glycogenolysis, glucagon is ineffective in glycogen-depleted individuals (e.g., those with alcohol-induced hypoglycaemia). Glucagon also stimulates insulin secretion and is therefore less useful in type 2 diabetes mellitus.