Treatment of type 1 diabetes mellitus
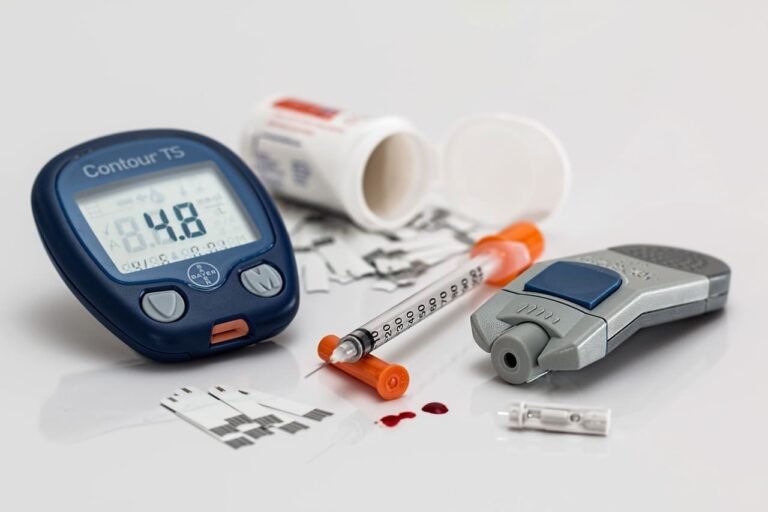
What is the treatment of type 1 diabetes mellitus?
Type 1 diabetes is treated with insulin from the time of diagnosis. Because individuals with type 1 DM partially or completely lack endogenous insulin production, administration of basal insulin is essential for regulating glycogen breakdown, gluconeogenesis, lipolysis, and ketogenesis. Likewise, insulin replacement for meals should be appropriate for the carbohydrate intake and insulin sensitivity, promoting normal glucose utilization and storage.
What are the preparations for insulin?
- Short acting insulin: also known as unmodified (‘soluble’ or ‘regular’) insulin is clear in appearance and more rapid absorption, onset of action and a shorter duration of action which allow greater flexibility as they can be injected closer to mealtimes (ideally 15–30 minutes before), and also associated with a decreased number of hypoglycemic episodes, primarily because the decay of insulin action corresponds to the decline in plasma glucose after a meal.
- Long-acting insulin: The onset of action of long-acting insulin is later and the duration of action is longer to avoid the frequent painful injections.
- Combined insulin: This type of insulin is a combination of short acting insulin with long acting insulin in an attempt to mimic physiologic insulin release with meals, particularly for individuals with type 2 diabetes with regular mealtimes who wish to avoid injecting more than twice a day.

What are the methods of insulin administration?
- Intermittent subcutaneous insulin injection: Insulin is most commonly administered several times a day as an injection into the subcutaneous adipose tissue of the anterior abdominal wall, upper arms, or outer thighs with the needle sited at a right angle to the skin.
- Continuous subcutaneous insulin infusion (insulin pump): CSII is a system of insulin delivery that uses a battery-operated medical device to deliver insulin continuously to people with type 1 diabetes. A variety of insulin pumps are available and the choice is often framed by cost, compatibility with CGM systems, and the personal preference or circumstances of the person with diabetes.
- Intravenous insulin therapy: Used in the management of hyperglycaemic emergencies and in stabilising blood glucose in a perioperative situation or unwell individuals, e.g. with poor oral intake or delayed gastric emptying.
- Inhaled insulin: Delivered via an inhaler into the lungs (e.g., Afrezza) but not suitable for smokers and for people with lung diseases like asthma or COPD but rarely used unless subcutaneous absorption is compromised.
What are the factors affecting the absorption of insulin?
- The site, depth, and volume of injection
- skin temperature (warming)
- exercise
- Accidental intramuscular injection results in more rapid absorption and hypoglycaemia it is more likely to occur in children and slim adults (with little subcutaneous adipose tissue)
- Lipohypertrophy causes delayed absorption of insulin which can develop at overused injection sites It can be avoided by not injecting into the same place.
What are the complications of insulin therapy?
- hypoglycaemia
- weight gain
- peripheral oedema
- insulin antibodies
- local allergy (rare)
- lipohypertrophy or lipoatrophy at injection sites