Treatment Of Type 2 Diabetes Mellitus
What is the treatment of type 2 diabetes mellitus?
The treatment of type 2 diabetes involves dietary, lifestyle advice, and exercise. Adding oral glucose-lowering agents, insulin, and other agents that improve glucose control is required at an early stage for those who have symptomatic hyperglycaemia or a high HbA1c. In addition to that, attention should be given to treating conditions associated with type 2 DM (e.g, obesity, hypertension, dyslipidemia, Cardiovascular diseases) and detection and management of DM-related complications.
What are the types of oral glucose-lowering agents?
- Biguanides
Metformin only biguanide available are widely used as first-line therapy for type 2 diabetes that causes modest sustained weight loss (on average 1–2 kg), does not cause hypoglycaemia, and has established benefits in micro-vascular disease and reducing the risk of myocardial infarction. Metformin is usually introduced at a low dose (500 mg twice daily) to minimise the risk of gastrointestinal side effects. The usual maintenance dose is 1000 mg twice daily (maximum licensed dose 1000 mg three times daily).
Mechanism of action: Metformin reduces hepatic glucose production, increases insulin mediated glucose uptake (insulin sensitiser), and has effects on gut glucose uptake and utilisation.
Side effects: Bloating, nausea, diarrhoea and abdominal pain, lactic acidosis, and vitamin B12 deficiency.
Contraindications: Metformin should not be used in patients with moderate renal insufficiency (glomerular filtration rate [GFR] <30 mL/min), any form of acidosis, unstable congestive heart failure (CHF), liver disease, or severe hypoxemia. Metformin should be discontinued in hospitalized patients, in patients who can take nothing orally, and in those receiving radiographic contrast material. Insulin should be used until metformin can be restarted
- Sulphonylureas
(glibornuride, gliclazide, gliburide) are short-onset of action insulin secretagogues that lower postprandial glucose by promoting pancreatic β-cell insulin secretion. Often used as an add-on to metformin, if glycaemia is inadequately controlled on metformin alone. Similar to metformin, the long-term benefit of sulphonylureas in reducing rates of microvascular complications was established in the UKPDS.
Mechanism of action: Sulphonylureas act by closing the pancreatic β cell ATP-sensitive potassium (KATP) channel, decreasing K+ efflux, and triggering insulin secretion by a series of molecular events.
Side effects: Hypoglycaemia especially in the elderly and weight gain.
Contraindications: Most sulphonylureas are metabolized by the liver and some of them by the kidney so they should be avoid in renal and liver insufficiency.
- Insulin secretagogues non-sulphonylureas
(mitiglinide, repaglinide, nateglinide) have similar action to sulphonylureas drugs.
- Alpha-glucosidase inhibitors
(acarbose, miglitol, voglibose) reduce postprandial hyperglycemia by delaying glucose absorption; they do not affect glucose utilization or insulin secretion. This type of oral glucose-lowering agent is not as potent as other oral agents in lowering the HbA1c but is unique because it reduces the postprandial glucose rise.
Mechanism of action: Reduce glucose absorption by inhibiting the enzyme that cleaves oligosaccharides into simple sugars in the intestinal lumen.
Side effect: The major side effects (diarrhea, flatulence, abdominal distention) are related to increased delivery of oligosaccharides to the large bowel and can be reduced somewhat by gradual upward dose titration. In addition to that, they also elevate liver function tests.
Contraindications: should be avoided in use with sulphonylureas because they increase levels of sulphonylureas and increase the incidence of hypoglycaemia. Simultaneous treatment with bile acid resins and antacids should also be avoided. These agents should not be used in individuals with inflammatory bowel disease, gastroparesis, or a serum creatinine >177 µmol/L (2 mg/dL).
- Thiazolidinediones
(pioglitazone, rosiglitazone) their use declined with the advent of other agents with fewer adverse effects and greater efficacy. Rosiglitazone was withdrawn from the market due to a subsequently disproven concern that it might increase rates of myocardial infarction. Pioglitazone remains in use and may reduce hepatic steatosis and NASH (nonalcoholic steatohepatitis) as well as providing protection from stroke.
Mechanism of action: Thiazolidinediones reduce insulin resistance by binding to the peroxisome proliferator-activated receptor γ (PPAR-γ). The PPAR-γ receptor is found at highest levels in adipocytes but is expressed at lower levels in many other tissues. Agonists of this receptor regulate a large number of genes, promote adipocyte differentiation, reduce hepatic fat accumulation, and promote fatty acid storage increasing fat mass and body weight.
Sideeffects: Thiazolidinediones are associated with weight gain(2-3kg) which fracture According to an FDA review pioglitazone may be associated with an increased risk of bladder cancer.
Contraindications: Thiazolidinediones are contraindicated in patients with hepatic insufficiency or CHF (class III or IV). The FDA has issued an alert that rare patients taking these agents may experience a worsening of diabetic macular edema. An increased risk of fractures has been noted in postmenopausal women taking these agents. Women should be warned about the risk of pregnancy because the safety of thiazolidinediones in pregnancy is not established.
- DPP-4 inhibitors
(sitagliptin, linagliptin, alogliptin, vildagliptin, saxagliptin) are all well tolerated and have a neutral effect on weight, but provide only moderate glucose-lowering activity. They are safe but do not improve cardiovascular outcomes. The DPP-4 inhibitors are useful in combination with other drugs to get HbA1c to target when it is only modestly elevated and are commonly used in older people as they have few adverse effects.
Mechanism of action: Inhibit dipeptidyl peptidase 4 (DPP-4) enzyme which is needed to break down GLP-1 and GIP (gut hormones that potentiate post-prandial insulin secretion) so enhance their circulating concentrations.
Side effects: Allergy, including rash, hypersensitivity reactions (including anaphylaxis, angioedema, and Stevens-Johnson syndrome), and severe joint pain have been reported in association with DPP-IV inhibitors.
Contraindications: should be caution in use in patients with renal insufficiency.
- GLP-1 receptor agonists
(liraglutide, semaglutide, and dulaglutide) reduce rates of major cardiovascular adverse events and cause weight loss, appetite suppression, and do not cause hypoglycaemia. Because this agent expensive compared with other agents, guidelines in the UK recommend that they should only be used third-line, as add-on therapy with other agents and only in those with a BMI of >30 kg/m2 (Scottish Intercollegiate Guideline Network, SIGN) or even 35 kg/m2 (National Institute for Health and Care Excellence NICE).
Mechanism of action: GLP-1 receptor agonists increase glucose-stimulated insulin secretion, suppress glucagon, slow gastric emptying, and induce satiety.
Side effects: The main side effect of GLP-1 receptor agonists is nausea, and they also increase the risk of acute pancreatitis.
Contraindications: GLP-1 receptor agonists should be avoided in patients with pancreatic disease or with other significant risk factors for acute pancreatitis (e.g., heavy alcohol use, severely elevated serum triglycerides, hypercalcemia).
- SGLT2 inhibitors
(dapagliflozin, empagliflozin, canagliflozin) are effective oral glucose-lowering agents that are usually added to other agents second-line treatment after metformin. They help with body weight reduction and are associated with improvements in cardiovascular and renal outcomes that have substantially advanced the treatment of type 2 diabetes.
Mechanism of action: Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors lower the blood glucose by selectively inhibiting this co-transporter, which is expressed in the proximal, convoluted tubule in the kidney. This inhibits glucose reabsorption, lowers the renal threshold for glucose, and leads to increased urinary glucose excretion. The loss of urinary glucose may promote modest weight reduction. Since these agents also impair proximal reabsorption of sodium, their use is associated with a diuretic effect and a 3–6 mmHg reduction in systolic blood pressure.
Side effect: Urinary and genital mycotic fungal) Infections are common in both men and women due to the increased urinary glucose. Polyuria and dehydration due to the diuretic effect can lead to reduced intravascular volume and acutely impaired kidney function. Euglycaemic diabetic ketoacidosis (i.e. DKA not associated with marked hyperglycaemia) is a rare complication of this type of drug, due insulin: glucagon ratio and consequent increased levels of circulating ketones.
Contraindications: These agents should not be prescribed for patients with type 1 DM or pancreatogenic forms of DM associated with insulin deficiency. It should also be avoided in moderate renal insufficiency.
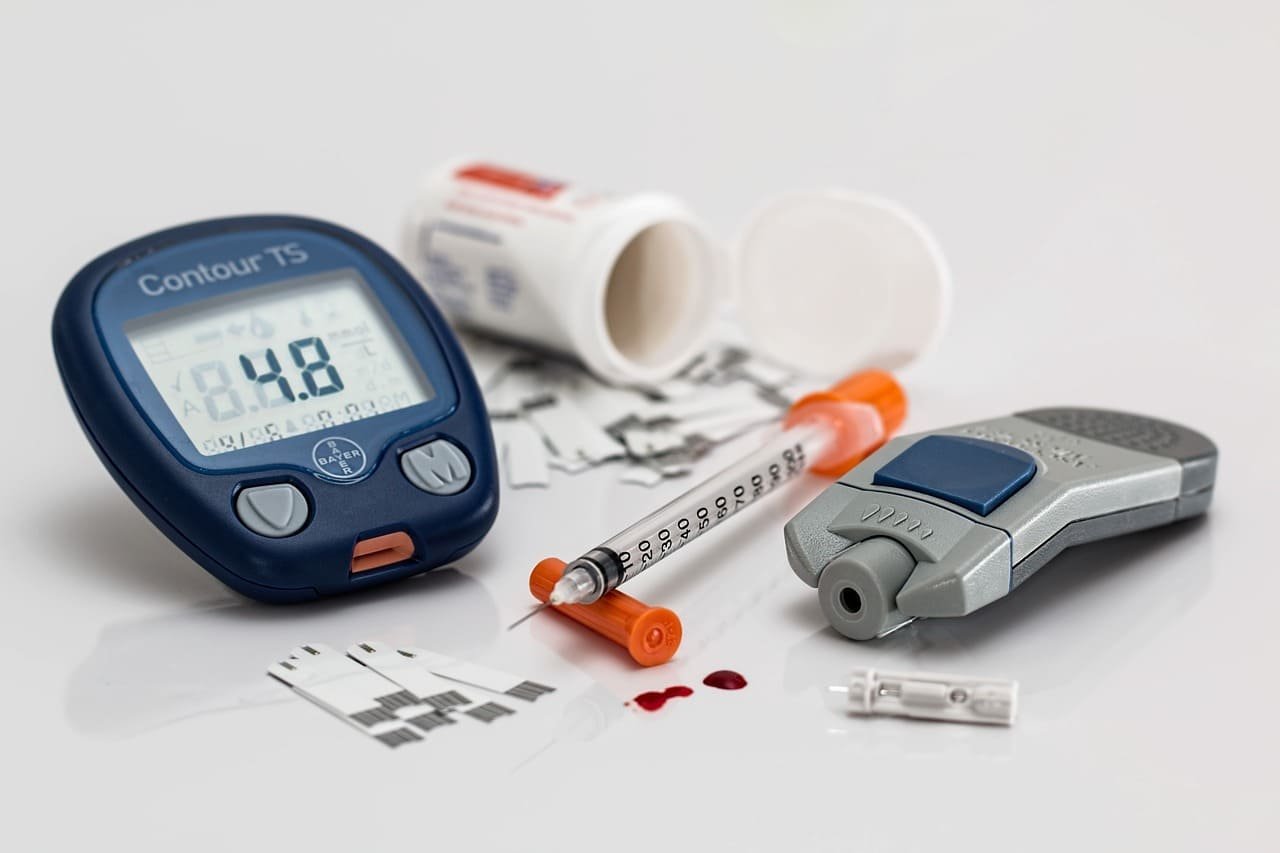
What is the rule of insulin in the treatment of type 2 diabetes?
The use of insulin in people with type 2 diabetes has been moved to later stages of the disease, as add-on therapy to other anti-diabetes agents because of the progressive nature of the disease and the relative insulin deficiency that develops in patients with longstanding diabetes. However, in case of obvious signs of catabolism, such as unintentional weight loss, an HbA1c higher than 10% (86mmol/mol), or glucose levels higher than 300mg/dl (16.7mmol/l), insulin should be considered without delay.